Mix up PHI and PII regulations, and you're gambling with million-dollar penalties.
These aren't just similar acronyms - they're entirely different data categories with their own legal landmines. PHI (Protected Health Information) lives under HIPAA's strict umbrella. PII (Personally Identifiable Information) covers everything that identifies someone, with rules that vary wildly depending on industry and location.
Most organizations get this wrong, treating all sensitive data the same way. This article exposes the critical differences between PHI and PII that keep compliance officers awake at night, reveals which protection strategies actually work, and shows how automated tools can eliminate the most common (and costly) security mistakes.
Difference between PII and PHI: Key distinctions for regulatory compliance
To protect sensitive information effectively, organizations must first understand exactly what they're protecting. The differences between PHI and PII determine which regulations apply, what protection measures are required, and what penalties you might face for mishandling them.
What is PHI?
Protected Health Information (PHI) includes medical details that can identify an individual and are created, used, or shared in the context of healthcare services. Under HIPAA, there are 18 specific identifiers classified as PHI:
- Personal Details: Patient names, birthdates, Social Security numbers
- Contact Information: Phone numbers, email addresses, fax numbers
- Geographic Data: Street addresses, ZIP codes (smaller than state)
- Health-Specific: Medical record numbers, health plan beneficiary numbers
- Digital Identifiers: Device serial numbers, IP addresses, website URLs
- Biometric Data: Finger and retinal prints, full-face photos
What is PII?
Personally Identifiable Information (PII) refers to any data that can be used to identify or locate someone. This includes both traditional identifiers and digital data:
- Direct identifiers: Social Security numbers, driver's license numbers, passport information
- Contact information: Phone numbers, email addresses, physical addresses
- Digital identifiers: IP addresses, login credentials, device identifiers
- Biometric data: Fingerprints, facial recognition data, voice patterns
PII is governed by regulations like GDPR, CCPA, and various state laws. The National Institute of Standards and Technology (NIST) has even created "PII Confidentiality Impact Levels" to evaluate the potential harm caused by unauthorized disclosure.
While PII covers a wide variety of personal data, PHI focuses on health-related information and requires even stricter protections.

PHI vs PII: Practical differences for compliance
How PHI and PII appear in real-world documents
Understanding how PHI and PII data types manifest in everyday documents helps organizations identify what needs protection:
Legal sector
- Court filings: May contain both PII (SSNs, addresses) and PHI (medical conditions disclosed in personal injury cases)
- Discovery documents: Often contain extensive PII that requires careful review before production
- Legal correspondence: May inadvertently contain client PHI when discussing healthcare-related matters
Healthcare industry
- Claims forms: Contain both PHI (diagnosis codes, treatment information) and PII (patient demographics)
- Medical records: Comprehensive PHI including treatment notes, test results, and patient identifiers
- Insurance communications: Include PHI (procedure codes, dates of service) with PII (subscriber information)

Government agencies
- Public records: May contain PII that needs redaction before FOIA release
- Program applications: Often include extensive PII (income verification, identifying documents)
- Investigation reports: May contain both PHI and PII, especially in health-related investigations
Financial services
- Loan applications: Contain extensive PII including financial account numbers and income details
- Account statements: Include PII that could be PHI when related to health savings accounts
- Insurance claims: May include both financial PII and health-related PHI
Get the PHI vs. PII classification wrong, and you're applying the wrong regulatory rulebook to your data. That mistake has cost companies millions in fines and turned routine audits into existential threats.
Is PHI a form of PII?
PHI is technically a specialized subset of PII—but this relationship creates more confusion than clarity in compliance contexts.
All PHI qualifies as PII because it identifies individuals. However, PHI carries additional legal protections under HIPAA that don't apply to other forms of PII. A patient's Social Security number in a medical record isn't just PII—it's PHI subject to HIPAA's stricter requirements.
The overlap creates compliance complexity
When the same data element appears in different contexts, it may be governed by different regulations:
- Medical context: A Social Security number in a patient file is PHI under HIPAA, requiring covered entity protections, business associate agreements, and specific breach notification procedures.
- Employment context: The same Social Security number in an HR file is PII under state privacy laws or employment regulations, with different protection requirements and breach notification timelines.
- Financial context: That Social Security number on a loan application becomes financial PII under GLBA or state financial privacy laws.
This means organizations handling health-related data must often comply with both HIPAA (for the PHI aspects) and other privacy regulations (for the broader PII elements). Healthcare organizations frequently make the mistake of assuming HIPAA compliance covers all their privacy obligations—it doesn't.
Why the distinction matters legally
Courts and regulators don't accept "it's all just personal data" as a defense. In enforcement actions, they evaluate whether you applied the correct regulatory framework to each data type. Treating PHI as generic PII typically results in inadequate protections and regulatory violations.
The most expensive compliance failures occur when organizations apply PII protection standards to PHI, assuming they're equivalent. HIPAA's technical safeguards, administrative requirements, and breach notification rules exceed most PII protection standards—and regulators enforce these differences aggressively.
Does PHI require more protection than PII?
PHI requires significantly stronger protections than most forms of PII, with more prescriptive requirements and harsher penalties for violations.
HIPAA's comprehensive protection framework
PHI protection under HIPAA involves three integrated rules that exceed typical PII protection requirements:
- Privacy Rule: Establishes detailed standards for PHI use and disclosure, including minimum necessary requirements and individual rights that go beyond most PII regulations.
- Security Rule: Mandates specific administrative, physical, and technical safeguards. These aren't suggested best practices—they're legal requirements with detailed implementation specifications.
- Breach Notification Rule: Requires notification to affected individuals without unreasonable delay and no later than 60 days after breach discovery, plus HHS reporting and potential media notification for breaches affecting 500+ individuals.
Stricter penalties and enforcement
HIPAA violations carry penalties up to $2.1 million annually per violation category, with criminal penalties including imprisonment. Most PII violations result in civil penalties and regulatory action, but rarely criminal prosecution.
The enforcement approach also differs significantly. HHS Office for Civil Rights conducts proactive compliance reviews and investigates every breach report. Most PII regulations rely primarily on complaint-driven enforcement.
Enhanced technical requirements
PHI demands stronger technical protections than typical PII:
Encryption requirements: HIPAA requires "addressable" implementation of encryption, meaning organizations must assess risk and adopt suitable encryption standards where feasible for data at rest and in transit. Many PII regulations recommend encryption but don't mandate risk-based implementation requirements.
Access controls: HIPAA requires role-based access, automatic logoff, and unique user identification. Generic PII protection often lacks these granular requirements.
Audit controls: HIPAA mandates comprehensive logging of PHI access and modifications. Most PII regulations require less detailed audit trails.
Integrity controls: PHI must be protected against improper alteration or destruction through specific technical measures.
Business associate complexity
PHI protection extends beyond the covered entity to all business associates—vendors, consultants, and service providers who might access PHI. Each relationship requires formal agreements and ongoing oversight that exceed typical PII vendor management.
This means healthcare organizations must evaluate and monitor their entire supply chain for HIPAA compliance, while most PII regulations focus primarily on the data controller's direct obligations.
The additional protection requirements for PHI reflect the sensitive nature of health information and the potential for discrimination, stigmatization, and harm if disclosed inappropriately.
Regulatory frameworks and penalties: The high cost of non-compliance
HIPAA violations now trigger up to $2.1M fines. GDPR penalties can reach 4% of global revenue. In 2023 alone, regulators handed out $2.25 billion in privacy-related fines.Regulators aren't just writing rules - they're enforcing them aggressively. Recent years have seen record-breaking penalties, with single violations sometimes costing more than entire annual compliance budgets. Companies once confident in their "good enough" security now find themselves explaining their negligence in depositions.
Regulatory landscape for sensitive data protection
The protection of PHI and PII is governed by overlapping regulations, each with specific requirements and enforcement mechanisms:
*NOTE: Only the most severe violations reach this cap; most are capped at $25k, $100k, or $250k under OCR discretion.
How HIPAA violations are categorized and penalized
The OCR applies a tiered penalty structure for HIPAA violations based on culpability:
Between April 2003 and March 2021, the OCR resolved 259,972 HIPAA complaints and imposed total penalties exceeding $135 million, demonstrating aggressive enforcement of these standards. Enforcement discretion caps exist for Tiers 1–3.
How violations typically occur
Most regulatory violations stem from preventable errors and oversight:
Technical failures
- Inadequate access controls: Failing to implement role-based access restrictions for sensitive information
- Transmission security gaps: Sending unencrypted PHI or PII via email or unsecured channels
- Insufficient audit tracking: Lacking systems to monitor who accessed sensitive data and when
Administrative oversights
- Incomplete risk assessments: Failing to identify where PHI and PII exist across systems
- Documentation deficiencies: Missing policies, procedures, or evidence of compliance efforts
- Training gaps: Staff unaware of proper protocols for handling sensitive information
Procedural breakdowns
- Improper document handling: Failing to properly secure sensitive information before sharing
- Business associate management: Inadequate vendor agreements or oversight
- Breach response failures: Delayed notification or inadequate remediation after incidents
Recent enforcement actions highlight how these failures lead to significant penalties:
"In 2024, Montefiore Medical Center was fined $4,750,000 for multiple HIPAA Security Rule Failures impacting 12,517 individuals".
Similarly, in the PII realm, Sephora's $1.2 million CCPA settlement demonstrated the serious consequences of privacy violations even outside healthcare contexts.
The increasing regulatory scrutiny across industries underscores why organizations must implement comprehensive strategies for protecting both PHI and PII—including secure processes for handling sensitive documents throughout their lifecycle.
How to protect PHI and PII effectively
To tackle the risks tied to sensitive data, combining technology, structured processes, and well-trained personnel is key. With healthcare breaches averaging $10.93 million per incident in 2023, it's clear that strong protective measures are non-negotiable.
Security measures for comprehensive protection
A layered security approach strengthens data protection. Here are some key controls:
Automated data redaction: The key to compliance
AI-powered redaction tools are a game-changer for safeguarding sensitive information. These tools can automatically detect and remove PHI and PII from various documents. Their standout features include:
- OCR (Optical Character Recognition) for processing scanned documents
- Pattern recognition to identify sensitive data formats
- Metadata scrubbing to eliminate hidden data
- Audit trails for tracking changes
- Version control to manage document updates
While these tools are effective, they work best alongside additional security measures for a multi-layered defense.
Employee guidelines for PHI and PII handling
Well-trained employees are your first line of defense. Establish clear policies and provide comprehensive training to minimize human errors.
Security awareness training
- Keep employees informed about evolving cyber threats
- Train staff to recognize and report suspicious activity
- Ensure they understand compliance requirements
Access control policies
- Enforce strict password management protocols
- Prohibit sharing of credentials among employees
- Update access rights promptly when job roles change
Documentation practices
- Record all data handling procedures in detail
- Maintain logs of security incident responses
- Keep track of completed training sessions
Additionally, organizations should offer anonymous reporting channels for potential violations, ensuring that any sensitive information within these reports remains secure. Regularly reviewing and updating policies helps keep defenses strong as new threats emerge.
The critical risks of PHI and PII exposure: Why proper protection matters
Healthcare data breaches now cost $9.77 million per incident. Legal firms lose clients overnight after privacy failures. Government agencies face public humiliation and leadership overhauls when sensitive data leaks.
This isn't theoretical. Organizations that mishandle PHI and PII face bankruptcy-level fines, criminal charges against individual employees, and permanent reputation damage that no PR campaign can fix.
Financial consequences of inadequate protection
When sensitive data isn't properly secured, the financial impact can be staggering:
- Healthcare breaches cost an average of $9.77 million per incident in 2024
- HIPAA violations can result in penalties up to $1.5 million annually per violation category
- Criminal penalties for willful HIPAA violations include fines up to $250,000 and imprisonment for up to 10 years
- Under GDPR, PII violations can cost organizations up to €20 million or 4% of global revenue
- CCPA violations can result in statutory damages of $100 to $750 per consumer per incident, and administrative fines up to $7,500 for intentional violations.
Real-world consequences that can't be undone
The fallout from PHI and PII exposure extends far beyond immediate financial penalties:
- Anthem Inc.'s 2015 breach exposed 78.8 million individuals’ health information, resulting in over $64 million in federal and state penalties, plus additional settlements
- Memorial Hermann Health System paid $2.4 million after improperly disclosing PHI to the media
- Montefiore Medical Center was fined $4.75 million in 2024 for HIPAA Security Rule failures affecting just 12,517 individuals
- A healthcare worker faced five years of probation and employment restrictions following unauthorized access to PHI
- Sephora paid $1.2 million for CCPA violations related to consumer PII

Common protection failures that lead to penalties
Organizations frequently fall into these preventable security traps:
- Visual privacy illusions: Believing sensitive information is protected when it isn't actually removed from documents
- Metadata oversight: Failing to address hidden document metadata containing personal information
- Manual process errors: Relying on time-consuming manual procedures prone to human error and inconsistency
- Inadequate audit trails: Lacking proper documentation of security activities required for compliance verification
- Insufficient collaboration controls: Using disconnected processes across teams, creating security gaps
The serious consequences of improper PHI and PII handling demonstrate why organizations need reliable, comprehensive data protection strategies. With regulations becoming increasingly strict, traditional methods simply can't meet compliance requirements or provide adequate protection against today's sophisticated threats.
How Redactable streamlines PHI and PII protection
Traditional redaction methods like black markers and basic PDF tools fail to provide permanent protection for sensitive information. Redactable transforms this error-prone, time-consuming process into an automated, reliable workflow that ensures complete removal of sensitive data.
Key benefits of Redactable for PHI and PII protection
- 98% time savings compared to manual redaction methods
- Permanent redaction that completely removes sensitive information, not just visual masking
- Guaranteed metadata removal to eliminate hidden personal information
- Browser-based accessibility for secure access from any device
- Detailed audit trails with redaction certificates for compliance verification
- Team collaboration features for secure document review across departments
How Redactable's AI-powered features address key challenges
Redactable offers multiple approaches to identify and protect sensitive information:
- Automated detection uses AI to find 30+ categories of sensitive data, including healthcare identifiers, financial information, and personal details
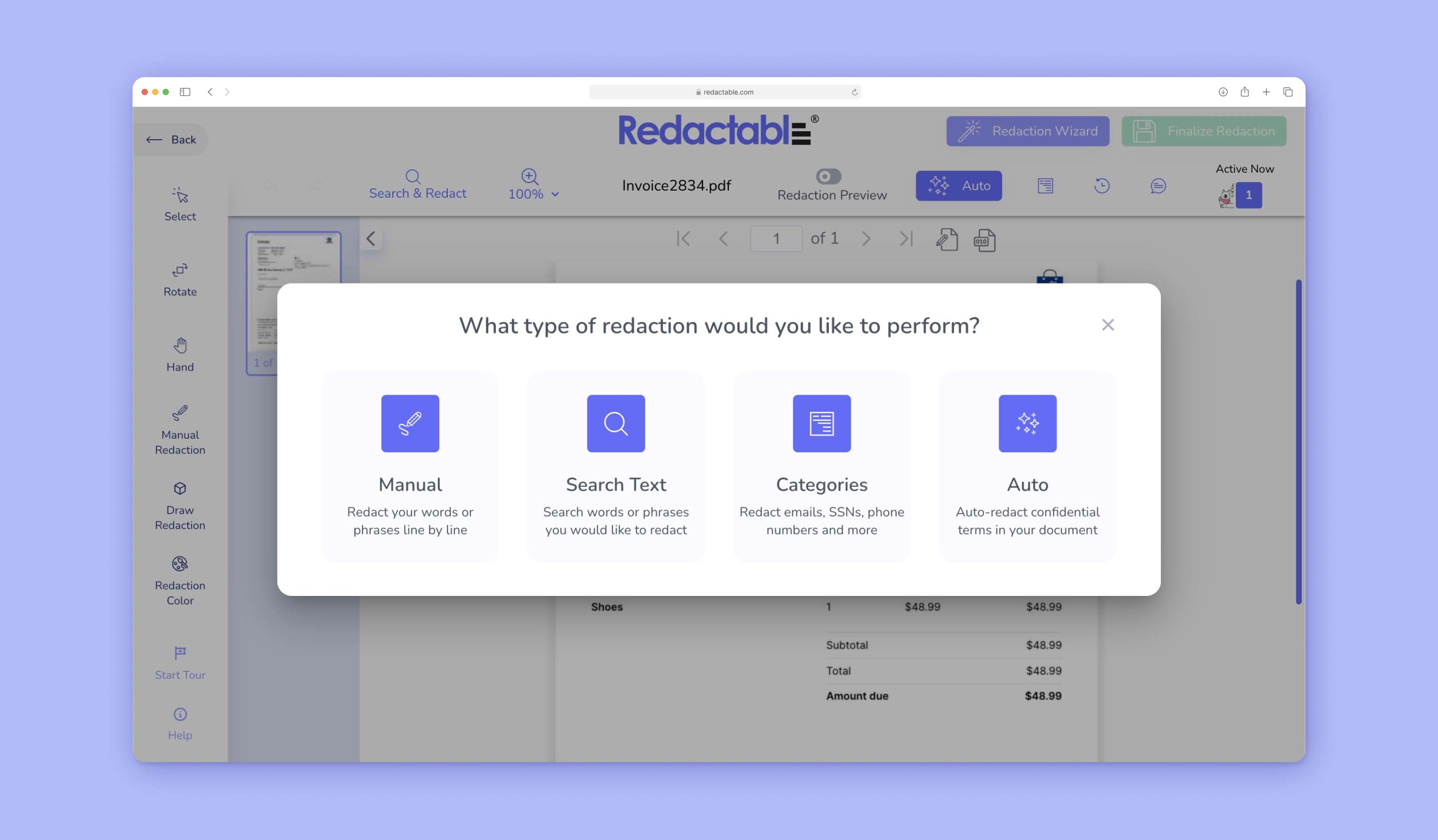
- Search & redact quickly locates specific terms or patterns across documents

- Manual redaction provides precise control for complex redaction needs
- Draw redaction allows redaction of images, charts, and non-text elements
Conclusion
PHI vs. PII isn't an academic distinction - it's the difference between compliance and catastrophe. The days of relying on black markers and basic PDF tools ended when regulators started handing out seven-figure fines for "unintentional" breaches.
Manual redaction often fails, leaving metadata traces and invisible text that auditors immediately flag. Redactable eliminates these risks automatically, permanently removing sensitive information while documenting your compliance efforts.
The math is simple: 98% time savings. Zero metadata leaks. Complete audit trails that satisfy even the strictest investigators.
Try Redactable for free today and discover why legal, healthcare, and government teams are abandoning outdated redaction methods before their next audit.







