Automated redaction software for RCM audit disclosures

Automated redaction software for RCM audit disclosures
Revenue cycle teams manage large volumes of sensitive documentation during payer and regulatory reviews: remittance files (EOBs/ERAs), claim forms (UB-04, CMS-1500), appeal packets, 835/837 attachments, coding sheets, and correspondence with auditors or vendors. Each of these records is filled with PHI that cannot be released without careful handling.
Redactable’s AI-powered platform ensures permanent removal of protected data not only the visible fields but also metadata, annotations, and hidden layers that standard tools often miss. With automation, healthcare organizations accelerate audit preparation, minimize compliance risk, and maintain patient privacy.
Instead of slowing down under manual review, revenue cycle staff can produce exactly what an auditor requires no more, no less while keeping disclosures defensible and free of PHI exposure.
How RCM audit requests are typically handled
Every payer or oversight body sets its own expectations for what must be produced. Most revenue cycle teams move through the following steps:
- Initial intake and review
Confirm the audit request is valid, identify the requesting entity, and record deadlines along with affected systems or facilities. - Gathering relevant documentation
Collect claims packets, coding worksheets, provider notes, attachments, and remittance files from EHR, billing, or document management platforms. - Determining disclosure boundaries
Assess which records are responsive, and mark portions containing PHI or proprietary details that require redaction. - Preparing production sets
Apply Bates numbers, assign privilege reasons where needed, and format documents to meet the auditor’s specifications. - Meeting submission deadlines
Deadlines often range from 14–45 days; extensions may be available but must be formally requested in advance.
Even when records fall within scope, PHI and PII cannot be disclosed directly. Permanent redaction is required to safeguard privacy and maintain HIPAA compliance.
Sensitive data commonly found in RCM audit packets
When preparing records for payer or RAC reviews, revenue cycle teams often encounter data points that cannot be shared without redaction. These elements pose the highest privacy and compliance risks.
Personal identifiers: Patient names, mailing addresses, phone and fax numbers, email addresses, Social Security numbers, medical record numbers, and insurance policy IDs.
Geographic and time details: Street-level addresses, postal codes, dates of birth, and admission, discharge, or service dates that could link back to an individual.
Financial references: Bank accounts, payment card data, and balance fields that are not essential to validating the audit scope.
Business-sensitive information: Reimbursement schedules, negotiated payer rates, and proprietary workflow documentation that fall outside disclosure requirements.
Visual or biometric markers: Faces, signatures, ID badges, and handwritten notes embedded in attachments or scanned forms.
When combined with claims or clinical data, these items are considered PHI under HIPAA. Redactable’s AI-driven platform automatically identifies and permanently removes them whether in documents, scanned packets, or images helping organizations deliver clean, compliant audit responses without privacy risk.
True redaction vs superficial masking

Black boxes or white overlays in standard PDF tools only cover content they don’t erase. Underlying text, metadata, or images can often be copied, pasted, or revealed with basic editing software. That’s not real redaction and leaves organizations exposed.
Redactable ensures permanent removal across all layers of a document:
- Sensitive text and numbers
Patient identifiers, account details, and PHI/PII are completely deleted, not just hidden. - Metadata and background layers
Properties, annotations, and embedded objects are stripped so nothing lingers in hidden fields. - Covered or transparent objects
Shapes, overlays, and masks are eliminated along with the data beneath them. - Embedded images and graphics
Visual identifiers faces, signatures, ID cards, or handwritten notes are securely erased and unrecoverable.
This process goes beyond cosmetic fixes, delivering HIPAA-ready files that withstand regulatory and legal scrutiny.
Steps to prepare RCM audit packets with confidence
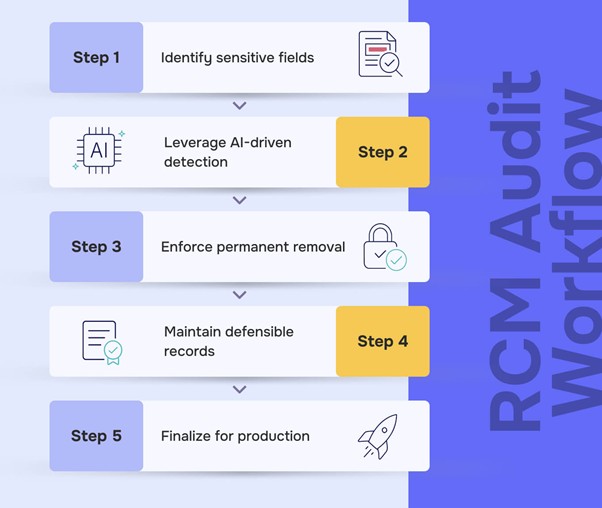
Revenue cycle and compliance teams face unforgiving audit timelines. Redactable helps eliminate manual bottlenecks by providing a clear, defensible process that ensures every disclosure is both accurate and HIPAA-compliant.
Identify sensitive fields
Review claims data, attachments, and correspondence for patient identifiers and financial details names, insurance IDs, MRNs, birth dates, and other information that could expose identity.
Leverage AI-driven detection
Use Redactable’s automated scanning to flag PHI and PII instantly. Staff can validate and adjust results, ensuring only the necessary information is redacted.
Enforce permanent removal
Go beyond black boxes. Redactable deletes text, metadata, hidden layers, and embedded visuals so no information can be recovered or reverse-engineered.
Maintain defensible records
Every action is captured in detailed logs. Generate certificates and privilege logs that show exactly what was removed, by whom, and when satisfying auditors and legal teams.
Finalize for production
Apply Bates numbers if required, lock in certificates, and export clean packets. Deliver responses on time with the assurance that no PHI slips through.
Redactable’s AI-driven platform for healthcare

RCM and compliance teams need redaction that keeps PHI secure while meeting tight production standards. Redactable is browser-based, HIPAA-ready, and integrates with the systems you already use.
Key features and benefits:
- Intelligent detection of sensitive data
Automated identification across 40+ categories: MRNs, patient/member IDs, SSNs, addresses, emails, face/signature detection, and financial details. - OCR for complex records
Converts scanned EOBs, faxed attachments, and image-based documents into searchable text for reliable redaction. - Multiple redaction modes
Auto-redaction, category filtering, keyword search, manual selection, and draw-box tools for tables and images. - Compliance and legal tools
Draft redactions, privilege log creation, Bates numbering, version history, and certified redaction reports. - Collaborative review
Role-based permissions, @mentions, threaded comments, and complete activity logs for cross-functional accountability. - Seamless integrations
Connects with Google Drive, OneDrive, Dropbox, Box, SharePoint, and Clio to streamline intake and production.
Enterprise-grade security
SOC 2 Type II, HIPAA support (with BAAs), CJIS alignment, and FIPS 140-2 validated encryption.
Interested in learning more?
Frequently asked questions
Any disclosures that contain PHI/PII claims forms, EOBs/ERAs, coding worksheets, appeal letters, payer correspondence, and embedded images must have identifiers removed unless specifically permitted.
Yes. Use Search Exclusions to retain claim/control numbers and redact member IDs, MRNs, and other high-risk identifiers.
By permanently removing sensitive data (not masking), cleansing metadata, and generating audit trails and certificates. Final compliance determinations remain with your organization.
Organizations risk PHI exposure, penalties, rework, and loss of payer trust. Permanent redaction plus certificates and logs provide defensible evidence.
Yes. OCR is built in scanned EOBs and legacy documents are recognized, then redacted with the same permanence.




.jpg)


