Patient identifiers are 18 specific types of information defined by HIPAA that can identify an individual in healthcare records. These HIPAA identifiers include names, Social Security numbers, addresses, phone numbers, and medical record numbers - data that healthcare organizations must protect or remove when sharing patient information.
Healthcare data breaches cost organizations an average of $7.42 million per incident as of 2025, down from previous years but still representing significant financial risk. Understanding what are patient identifiers under HIPAA isn't just regulatory compliance - it's financial protection against devastating fines and lawsuits.
What are the 18 HIPAA patient identifiers?
HIPAA defines exactly 18 patient identifiers that healthcare organizations must protect. This finite list determines what information requires redaction when sharing patient data for research, legal proceedings, or public records requests.
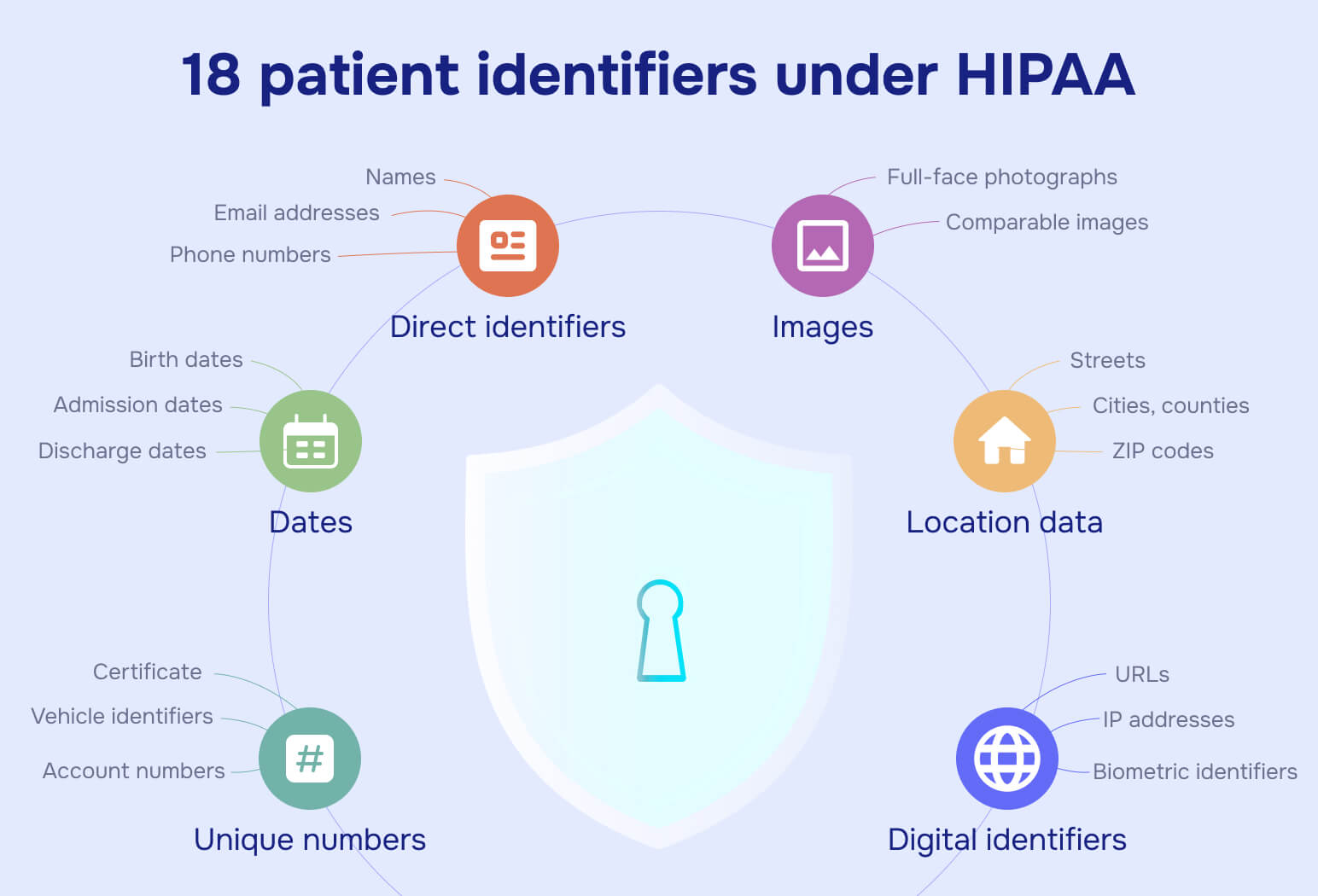
Below is the official patient identifiers list:
Direct identifiers
- Names (first, last, maiden)
- Social Security numbers
- Email addresses
- Phone numbers (all types)
- Fax numbers
Location data
- Street addresses
- Cities, counties, states
- ZIP codes (all digits)
- Geographic coordinates
Dates
- Birth dates
- Admission dates
- Discharge dates
- Death dates
- All other dates related to an individual
Unique numbers
- Medical record numbers
- Health plan beneficiary numbers
- Account numbers
- Certificate/license numbers
- Vehicle identifiers and serial numbers
- Device identifiers and serial numbers
Digital identifiers
- URLs
- IP addresses
- Biometric identifiers (fingerprints, voiceprints)
Images
- Full-face photographs
- Comparable images
These 18 categories cover any information that could reasonably identify a specific patient when combined with health data.
Which data is not a HIPAA identifier?
Understanding what doesn't qualify as a patient identifier helps healthcare organizations avoid over-redaction while maintaining compliance.
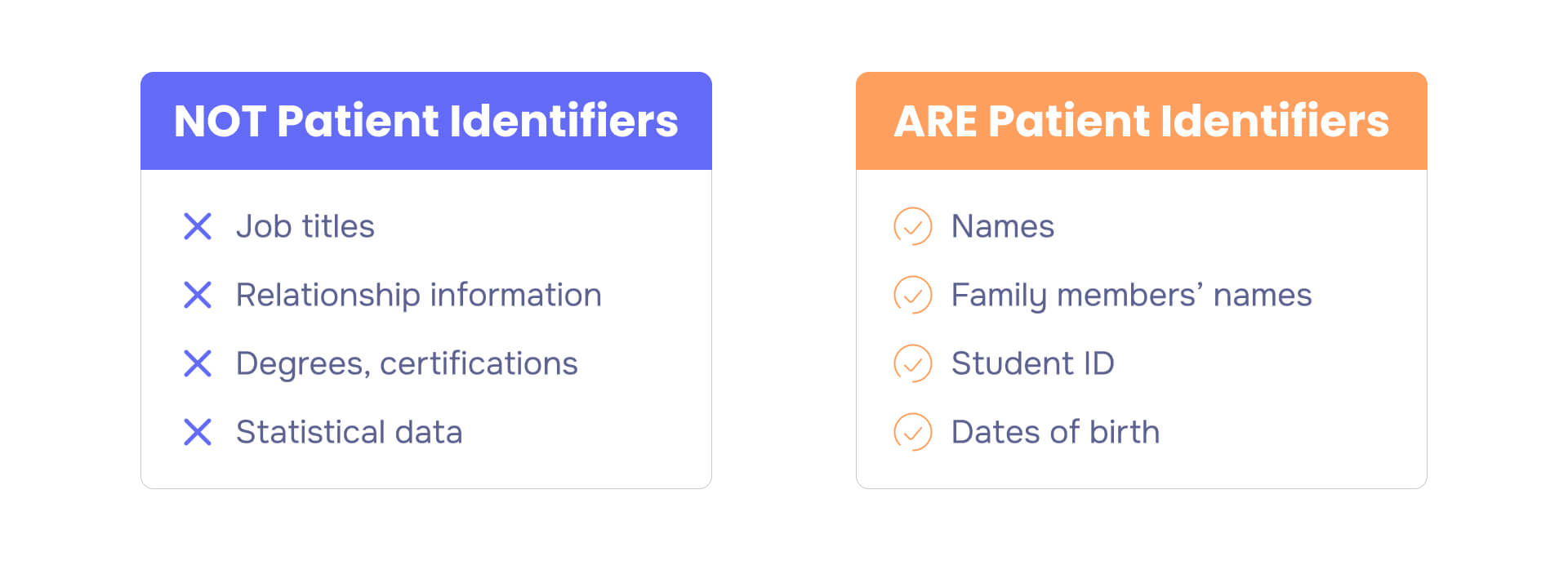
Data not considered patient identifiers:
Employment information: Job titles, employer names, and work status don't appear on the 18-identifier list.Example: "Software Engineer at Tech Company"
Marital status: Relationship information isn't a direct patient identifier under HIPAA. Example: "Married," "Single," "Divorced"
Educational background: Degrees, certifications, and schooling information fall outside the identifier list.Example: "Bachelor's Degree," "High School Graduate"
Statistical data: Aggregated information that cannot trace back to individuals isn't considered identifying.Example: "15% of patients experienced side effects"
De-identified health information: Once all 18 identifiers are properly removed, the remaining data no longer qualifies as protected health information.Example: Medical research datasets with only diagnoses and outcomes
HIPAA compliance checklist for patient identifiers
Immediate priority actions:
- Conduct comprehensive risk analysis focusing on patient identifier protection across all systems
- Implement multi-factor authentication for all systems containing patient identifiers
- Review patient access procedures ensuring compliance with Right of Access requirements
- Document training completion for all workforce members handling patient identifiers
Medium-term strategic improvements:
- Enhance workforce training programs with role-specific patient identifier handling content
- Strengthen business associate management through comprehensive agreement reviews
- Upgrade technical infrastructure with enhanced encryption and audit logging capabilities
- Establish incident response procedures with defined escalation paths
Long-term compliance planning:
- Prepare for upcoming Security Rule requirements by monitoring final rule development
- Develop advanced cybersecurity capabilities aligned with Performance Goals framework
- Establish continuous improvement processes through regular compliance assessments
What are acceptable patient identifiers for healthcare use?
Acceptable patient identifiers HIPAA serve different purposes depending on the healthcare setting. For treatment and internal operations, all 18 HIPAA identifiers can be used as needed for patient care. For research, quality improvement, and public health activities, healthcare organizations must follow specific de-identification standards.
Safe Harbor method: Remove all 18 HIPAA identifiers completely. This creates a "safe harbor" for data use without additional risk assessment.
Expert Determination method: A qualified expert determines that the risk of identifying patients from remaining data is "very small." This method allows retention of some identifying information when necessary for research validity.
HIPAA security and privacy rules for patient identifiers
Criminal activity, not accidents, drives most patient identifier breaches. Healthcare organizations face two core HIPAA requirements for protecting patient identifiers.
Privacy Rule requirements: Sets national standards for protecting patient identifiers in all formats. Gives patients control over their information and restricts how organizations can use or disclose identifying data.
Security Rule requirements: Establishes technical, administrative, and physical safeguards for electronic patient identifiers. Requires encryption, access controls, and audit systems for digital health information.
Both rules work together to ensure patient identifiers remain confidential while allowing necessary healthcare operations and research.
Read also: What are the three rules of HIPAA?
De-identification: Removing patient identifiers for research
De-identification removes patient identifiers from health records, enabling vital medical research while protecting privacy. Once properly de-identified, health information no longer falls under HIPAA restrictions.
Why de-identification matters
Six in 10 American adults have chronic diseases requiring ongoing research for better treatments. De-identification allows researchers to analyze large healthcare datasets without compromising patient privacy.
During COVID-19, privacy restrictions initially slowed research efforts. Proper de-identification processes eventually enabled rapid analysis of patient data, accelerating treatment development while maintaining confidentiality.
Public cases: The cost of exposing HIPAA patient identifiers
Healthcare organizations face severe financial consequences when patient identifiers are exposed inappropriately.
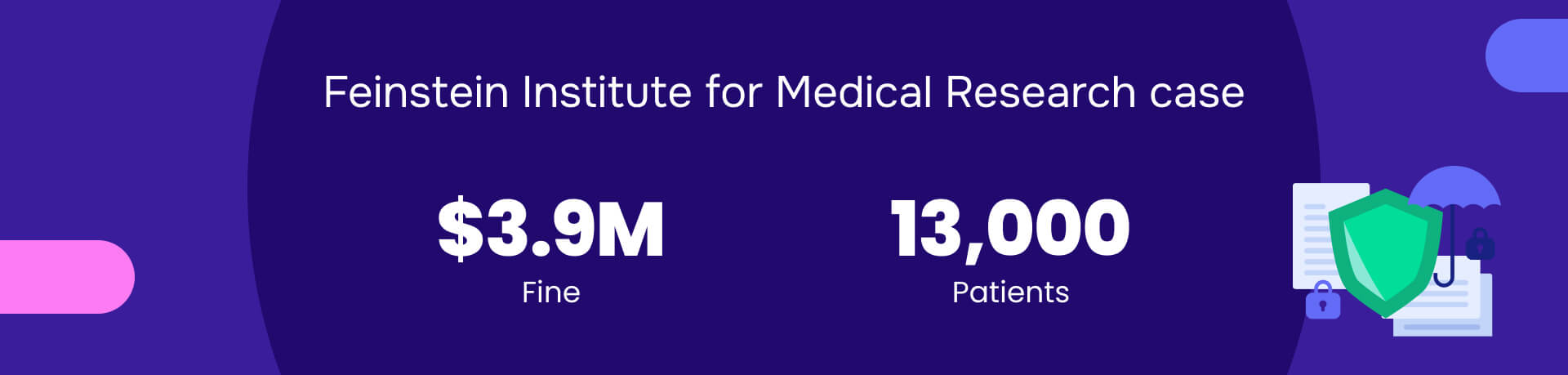
Feinstein Institute case: The Feinstein Institute for Medical Research paid $3.9 million after a laptop theft exposed patient identifiers for 13,000 research participants. This case demonstrates the liability of holding identifiable research data.
Industry response: Pharmaceutical companies now rely heavily on de-identified data:
- 70% of clinical trials use anonymized patient data from electronic health records
- Real-world evidence studies analyzed de-identified data from over 500 million patients in 2023
De-identification provides legal protection while enabling life-saving research.
2025 HIPAA enforcement priorities
Healthcare organizations face intensified regulatory scrutiny with new enforcement initiatives targeting specific HIPAA compliance gaps. Understanding current priorities helps organizations allocate resources effectively.
Risk Analysis Initiative results: HHS Office for Civil Rights launched a focused enforcement program in October 2024, resulting in eight settlements totaling nearly $900,000 within months. This initiative specifically targets organizations failing to conduct comprehensive, organization-specific risk assessments.
Recent major settlements demonstrate escalating penalties:

- Solara Medical Supplies: $3 million (January 2025) - 114,007 individuals affected by inadequate security controls
- Montefiore Medical Center: $4.75 million (February 2024) - malicious insider investigation failures
- Gulf Coast Pain Consultants: $1.19 million - unauthorized contractor access to 34,310 patients
Common enforcement themes include:
- Generic risk assessment templates instead of customized analyses
- Inadequate workforce training and sanctions policies
- Missing or ineffective business associate oversight
- Delayed breach notifications beyond 60-day requirements
Regulatory updates and future outlook
HIPAA Security Rule modernization: HHS published a Notice of Proposed Rulemaking in January 2025, representing the first major Security Rule update since 2013. Key provisions include:
- Technology asset inventory and network mapping requirements
- Enhanced cybersecurity controls aligned with industry frameworks
- Annual review requirements for all security measures
- Strengthened enforcement mechanisms for non-compliance
The comment period closes March 7, 2025, with final rule publication expected in 2026 and implementation dates 12-18 months thereafter.
Healthcare Cybersecurity Performance Goals: HHS introduced voluntary cybersecurity goals in January 2024 to strengthen sector resilience. While voluntary, these goals increasingly influence enforcement expectations and represent best practices for patient identifier protection.
Industry-specific implementation guidance
Different healthcare settings require tailored approaches to patient identifier protection based on their unique workflows and technical environments.
Hospitals and health systems
Complex multi-department workflows require sophisticated access controls reflecting clinical care patterns. Key considerations include:
- Role-based access controls supporting diverse clinical roles
- Integration security for medical devices and IoT systems
- Specialized training programs for different departments
- Comprehensive credentialing reviews tied to access privileges
Private practices and small provider
Cost-effective solutions enable compliance without extensive IT infrastructure investments:
- Cloud-based security services with appropriate business associate agreements
- HHS-provided templates and guidance materials adapted to practice size
- Simple but comprehensive policies and training programs
- Basic cybersecurity hygiene practices with automated monitoring tools
Research institutions
Unique de-identification challenges require specialized approaches:
- Formal expert determination processes for complex research datasets
- IRB coordination for PHI research authorization requirements
- Long-term data retention security protocols
- Comprehensive data use agreements with research partners
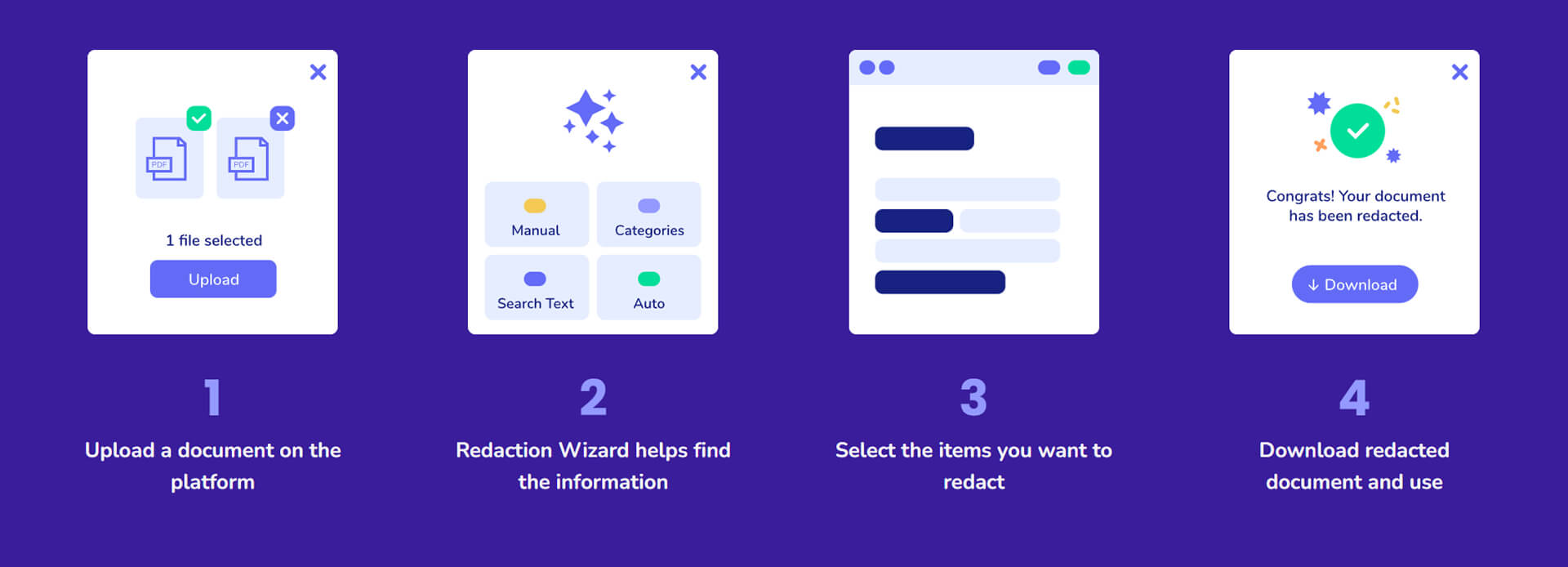
How Redactable protects patient identifiers
Manual redaction of patient identifiers creates liability through human error and incomplete removal. Redactable's AI-powered platform automatically identifies and permanently removes all 18 HIPAA identifiers with 98% time savings compared to manual methods.
Read also: HIPAA redaction: Best practices to prevent violations
Protecting patient identifiers with automated redaction
Healthcare organizations can protect patient identifiers through Redactable's systematic approach:
Document upload and encryption: Upload files directly to the secure platform. Documents receive immediate encryption, protecting patient identifiers from the moment they enter the system.
Automated identifier detection: AI algorithms scan documents and highlight all 18 HIPAA identifiers automatically. This eliminates the manual review process that creates compliance gaps.
Expert review and validation: Healthcare professionals can review AI suggestions and manually adjust redactions as needed. This step ensures accuracy for Expert Determination compliance while maintaining efficiency.
Permanent redaction and certification: Finalize redactions with permanent removal of patient identifiers. The platform generates compliance certificates documenting the redaction process for audit purposes.
Secure document delivery: Download clean documents with all patient identifiers permanently removed. Files are ready for research, legal discovery, or public records requests without HIPAA violations.
Healthcare organizations protecting patient identifiers need automated solutions that eliminate human error while ensuring regulatory compliance. Redactable's AI-powered software provides the speed, accuracy, and audit capabilities for HIPAA compliance.
Protect patient identifiers with 98% time savings - try Redactable free today!